 This blog begins my new journey of discovery pertaining to the Gastroc and Soleus muscles, my mild Achilles Tendinitis, a Short Leg Syndrome whether it be a Functional Limb Length Discrepancy and/or a true bone Structural Limb Length Discrepancy and how I’ve been affected in my pelvis all these years. This blog picks up chronologically where I left off in this last blog entitled: https://si-instability.com/post-high-ankle-sprain-tib-fib-surgery-great-to-be-walking-again-5-10-weeks-recovery-update/In the meantime I just posted a short final recovery update blog pertaining to the healing of my last Arthrex TightRope Fixation Surgery.
This blog begins my new journey of discovery pertaining to the Gastroc and Soleus muscles, my mild Achilles Tendinitis, a Short Leg Syndrome whether it be a Functional Limb Length Discrepancy and/or a true bone Structural Limb Length Discrepancy and how I’ve been affected in my pelvis all these years. This blog picks up chronologically where I left off in this last blog entitled: https://si-instability.com/post-high-ankle-sprain-tib-fib-surgery-great-to-be-walking-again-5-10-weeks-recovery-update/In the meantime I just posted a short final recovery update blog pertaining to the healing of my last Arthrex TightRope Fixation Surgery.
Now as I continue along:
Sept. 25th, 2014 – I went to my chiropractor, Dr. Sheldon, mainly for him to adjust my right elbow after a picture fell from wall and hit my muscles/tendons of medial forearm. In the appointment I asked him to manually palpate the motion of my left ankle and he said: “Her passive ROM in her left ankle is restricted on dorsiflexion and supination combined.” Dr. Sheldon was sharing his chiropractic findings which were similar to a foot doctor performing the Silfverskiöld Test as defined here: “The Silfverskiold test is the clinical standard for equinus. The practitioner begins by fully extending the knee. With the subtalar joint (STJ) in neutral, supinate the forefoot, dorsiflex the foot, and measure the angle of dorsiflexion at the ankle. Next flex the knee to 90 degrees and repeat the measurement.”
The quote above is taken from an article entitled and linked herein: “Equinus, By Séamus Kennedy, BEng (Mech), CPed” An excellent article in trying to understand the Equinus condition of the lower leg. By this time I had been constantly stretching many times during the day hoping to get relief.
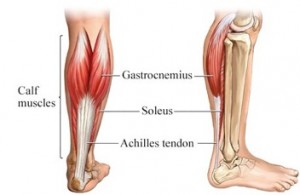
Oct. 16th 2014 – I made a trip back to my Dr. Gent of Kitsap Foot and Ankle Clinic as a post surgical follow up appointment and to transition into dealing with the pain of my non-insertional Achilles Tendinitis that had been concurrently going on with the high ankle sprain. It was difficult to sort out the 2 places of pain prior to my last surgery, but now it is so much easier when another piece of the puzzle has been taken care of. Here is a link to an article by the AAOS explaining the difference between insertional and non-insertional Achilles Tendinitis and protocol. I have no pain at my heel except for intermittent pain at lateral corner of top of heal where the tendon inserts. Most of my pain is located say 2 inches above the heal and also farther up where the Gastroc and Soleus muscles converge into the Achilles Tendon. My prior MRI on 9/6/13 a year ago showed Pre -Achilles Tendinitis of my left ankle. From my last blog, I had already been doing night stretching with the Ossur Night Splint. I’ve been in physical therapy weekly since August and constant stretching every day. The night splint was not comfortable at all and it would set off spasms up the back of my leg.
So at this appointment, Dr. Gent did a PRP (Platelet Rich Plasma) injection using the same company for preparing the injection as mentioned in this prior blog link. He injected PRP into the Gastroc-Soleal Aponeurosis Band ( meaning: A sheetlike fibrous membrane resembling a flattened tendon that serves as a fascia to bind muscles together or to connect muscle to bone.) A 2nd injection point was also done lower down at the now insertional portion of the achilles tendon. I was placed into a molded posterior splint to hold my ankle to 90 degrees to see if this would be more comfortable than the prior Ossur Splint. It was more comfortable especially when rolling over to my side at night from sleeping mainly on my back. Dr. Gent observed my walking gait and noted: There is a tight Achilles Left Tendon with the heel having an early heel lift in gait. Right Shoulder drop with right leg stride. There is a tightness that is accentuated with the knee extended vs bent. There is pain and cramping that is occurring into the calf muscle area that is compromising her healing and walking/standing activities.

After the posterior splint was molded/dried, I was transferred to my tall walking boot to leave his office. I was able to bear weight and used crutches for one day. I stayed close to the hotel room for 2 days before leaving to come back to Idaho. Regarding the PRP injections, Dr. Gent does a good job of numbing the area of injection and just minor pressure was felt during the injection. That night my leg ached and with one Hydrocodone 10/325 along with 1 Diazepam 5mg I was able to sleep. You cannot take anti-inflammatories after these kind of injections as it defeats the purpose of the inflammatory response that is normal to the injection. By the time I traveled home as pictured, I didn’t think much of the injection. I had no pain as I just needed the comfort of the walking boot for a few days. For more severe Achilles tears, a walking boot a/or crutches may be instituted for a longer period of time following these injections. My case was very mild with no tears. Dr. Gent mentioned a Gastroc Recession surgery on my left leg to achieve the Achilles lengthening that I needed should I not be able to achieve my goals conservatively. He wanted me to talk to him again in 2 weeks to see how I was doing after the injections and continued physical therapy.
During the last two weeks, I prepared myself with a lot of research pertaining to the Gastroc/Soleus complex and the bio-mechanics of the lack of dorsiflexion and its relationship to the Gastroc Equinus. Here are links to many excellent articles to read. The first link I also posted on my Facebook page as I was so impressed with what I had read that just rang volumes of hope and inspiration to me to figure out any remaining issues with my lower leg.
http://www.podiatrytoday.com/understanding-biomechanics-equinus
http://www.foothealthfacts.org/footankleinfo/Equinus.htm
http://www.aaos.org/news/bulletin/oct07/clinical4.asp
Here are links to surgery articles that I read in order to be prepared to ask questions the next time I talked to Dr. Gent pertaining to his possible surgical intervention:
EGRTechniqueGuide (Endoscopic Gastrocnemius Recession Technique Guide)
Gastrocnemius soleus recession a simpler, more limited approach
Oct. 28th, 2014 – I had my last rehab physical therapy appointment with Mark Bengtson, Pinnacle Physical Therapy. Other than continually increasing strength of all muscles connecting to the pelvis, I finally achieved the goal of understanding what it was to feel pelvic neutrality of my muscles after 3 1/2 years of Mark’s PRI-Postural Restoration Institute Training expertise. This was built upon a prior stabilized pelvis with my SI surgery and all the now stabilized lower extremity joints. Now that I could stand in true neutral and be fully aware of any compensation patterns in my lower back when walking, I had come to realize that the shortness/tightness of my left Gastroc and Soleus was demanding an altering of my gait to accommodate it. I told Mark how happy I was that I could feel what it meant to walk straight without any bend of my spine; yet to do so, I had to walk more on my midfoot and toes with left foot to avoid the pull or compensation that my right side wanted to shorten up to help the left side. Since Mark was working on behalf of Dr. Gent for my post surgical ankle rehab, he proceeded to have a conversation with Dr. Gent pertaining to my inability to lengthen my left calf in order to have a proper walking gait.
This is one of my favorite sites to read to get understanding of the relationship between our legs and pelvis. Here is an excellent, easy to understand article by Erik Dalton, PhD a Myoskeletal Therapist, regarding short legs and a crooked pelvis at this link: http://erikdalton.com/short-leg-syndrome-part-1/ This is just one of many wonderful articles on his site.
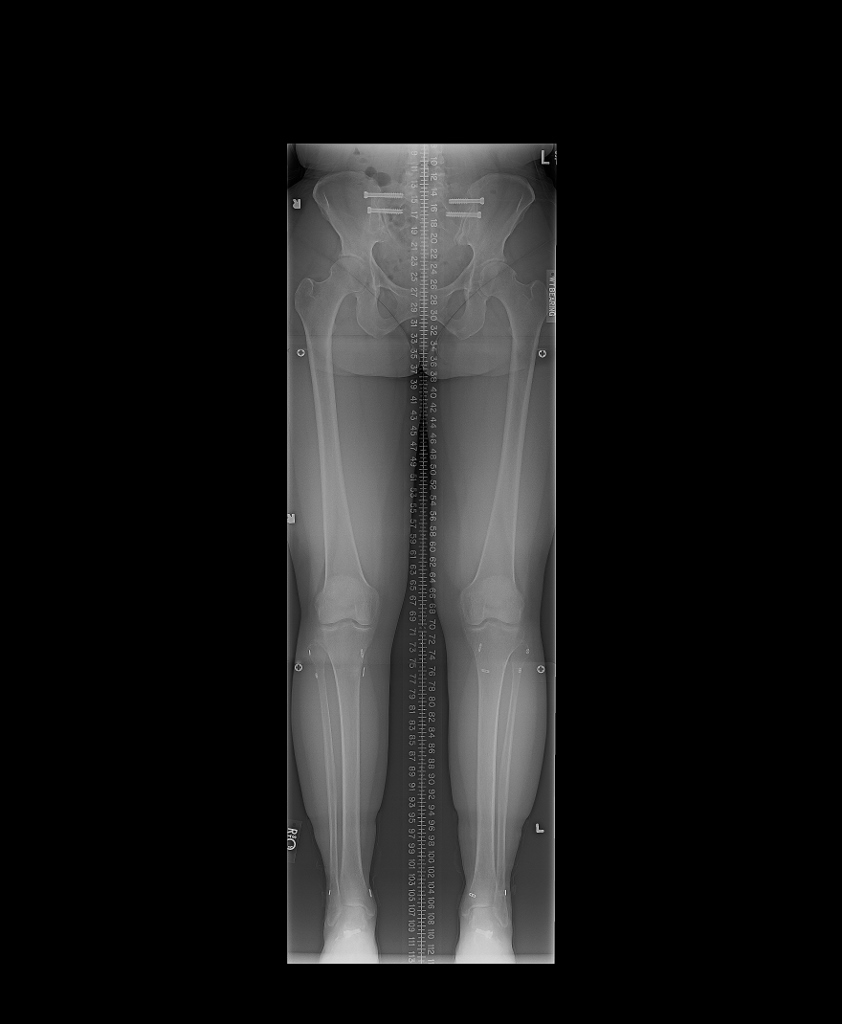
In this last week leading up to the writing of this blog, I’ve come to a grip with the fact that I’ve had a minor Equinus probably for my entire life that certainly could have lead the way in walking compensation patterns along with my flexibility and mild excessive pronation. This certainly could have been the beginning of the pelvis problems leading up to my SI Dysfunction to the point of needing surgery to stop that dysfunction in order to help preserve my lumbar spine. I was told from a child I had a higher right hip. To prove the point for ruling in or out true leg length discrepancy, I had the following limb length x-ray ordered by my sports physician, Dr. PZ Pearce of Champion Sports Medicine, Spokane.
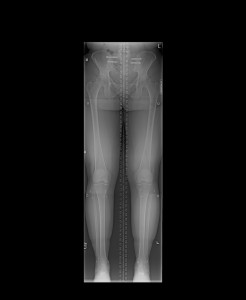
Oct. 28th, 2014 –(Click on image to enlarge) Inland Imaging Radiologist report findings: “The bone mineralization is within normal limits. The right leg measures 4mm longer than the left. No valgus or varus deformity is seen. There is a mild marginal hypertrophy from both hips. The femoral heads have smooth contour. The knee and ankle joints appear normal. There are 2 screws traversing each sacroiliac joint. There are post surgical changes with small cortical buttons and surgical tracts across the proximal and distal tibia and fibula.” Impression: “1. Right leg measures 4 mm longer than left, 2. Mild bilateral hip osteoarthritis.”
In my opinion, I found this report to be very helpful and relieving to me of the idea that I had a really longer right leg. Even though I now know that 4mm is a very tiny amount of bony leg difference, it still can be significant with some patients. I am dealing with both this and a muscular/tendon situation on the lower left leg. Also I was pleased to find out that nothing has changed in my hip joints themselves after the SI Surgery as I already had mild to moderate DJD of hips on CT scan in Nov. 2012 before the surgery as posted on my Chronological History page of my website.
Oct. 29th, 2014 -My local personal training consultant, Joanna Alford, PT helped me make the video below of my walking and showing exercises proving the point of shortness in my left calf more Gastroc but some Soleus influence. This video was uploaded for Dr. Gent to see my progress.
Oct. 30th, 2014 – To sum up my hour long phone appointment with Dr. Gent, Kitsap Foot and Ankle Clinic, Bremerton, WA, he sincerely appreciated the video that I sent him. He simply stated that there was no doubt that I do have the Gastroc/Soleus mild Equinus and he would offer me his surgical skill with the Endoscopic Gastroc/Soleus Recession. He used to do the open procedure but awhile back he learned the Endoscopic procedure when it first came out. He appreciated that I would trust and consider this surgical solution for my situation. He felt that this surgery offered a good outcome for mild Equinus patients with minimal surgical trauma. I asked if what I felt post surgically would be similar too my experience with my prior peripheral nerve decompression surgeries and he said yes. It is a similar concept of releasing fascia (Aponeurosis) that is currently constricting the Gastroc and Soleus muscles of the Superficial Posterior Compartment of my leg. If I understood him correctly, this would give a lengthening to the muscles and ability to stretch the Achilles and ultimately give me more dorsiflexion when walking along with calming down the spastic knots up back of my leg.
Nov. 5th, 2014 – I had the 2nd appointment with another Physical Therapist specializing in pelvic floor issues of women in regards to my intermittent piriformis syndrome. I will write about this more in a future blog. The point here is she had evaluated my gait and I quote the following objective finding from my chart note by Christy Frazier, DPT-Apex PT of North Spokane: “Limited left ankle Dorsiflexion causing the left knee excessive extension and pelvic rotation. Able to consciously correct this gait pattern.” Assessment: “Kim is experiencing signs and symptoms consistent with left medial thigh fascial restrictions which could be related to gait pattern.”
I share this finding to simply say I appreciate confirming information regarding my gait from now 3 physical therapists. When she said I could consciously correct the gait, that is true. By correcting my gait, I walk straight and no compensation/rotation of pelvis; however, to do this my left heel all the more so stays off the ground and I’m walking more on my toes which are the symptoms of Equinus. Yet if I walk correctly, no matter the increased pressure on the toes to do so, I have obviously less torque on my pelvis. Then my fascial symptoms which lead to burning sensations calm down. As soon as I try to walk say in and around a Costco store, I come out with fascial irritation of my medial thighs left greater than right as I cannot maintain walking correctly by being on my midfoot/toes. I will fall back to the compensated way of walking and I then stress my opposite right knee and ankle and increase fascial constrictions leading to burning sensations.
Nov. 6th, 2014 – I will return to Dr. Gent here in a few weeks for him to further discuss the surgical procedure and post op protocol with me along with answering my questions/concerns. My husband and I made the decision that I would take Dr. Gent’s advice and we are working on planning a surgical date. If I could, I’d have the surgery done by now but I want to get as much strength as I can in the pelvic/hip and thigh muscles with isolated exercise minus the walking. I also want the opportunity to dress up (minus the casts/splints/ or walking boots) for the holidays while singing in my annual vocal recital and Christmas Contadas. I’m grateful for the quality of life I have since a year ago and I’m willing to give that up temporarily to endure another post surgical rehab in order to gain the greater good of a better walking gait.
Nov. 10th, 2014 – I spent the past gloomy days reading all that I can pertaining to limb length discrepancy. Here is just one of many articles on the internet for this subject, a Blacktown Podiatry in Australia article: http://www.footproblems.com.au/foot-problems/leg-length-discrepancy.html
The reason for reading is for me to try and figure out how much 4mm affects my gait in and of itself separate from the mild Equinus of my calf muscles. As I researched, I also settled on this website as being very informative regarding the subject of heel lifts: http://clearlyadjustable.com/ After reading this site, I ordered the heel lift through this affiliated site: GW Heel Lift, Inc. I will have the product in time to take it to Dr. Gent for his review and determination of usage in my left shorter leg shoe. The lady at GW Heel Lift, Inc. was very helpful on the phone and concurred that the clearly adjustable heel lift product would be the best for my situation even though they do sell many other varieties of heel and full foot lifts. This product is adjustable to my exact 4mm discrepancy and is suppose to fit nicely under my normal shoe insert. Also in my reading it is important to know that correcting a long time leg difference could be met with some challenges. I am a very well tuned in patient and most likely I can figure this out on my own; yet I will continue my chiropractic care to see if there are any adverse effects of the heel lift with regards to my spine.
My patient to patient advice: Do not go out and get a heel lift without having the leg length x-rays and a medical professional working with you in the process. However, don’t delay in discovering for yourself if a limb length could be a contributing factor. Press in and ask questions even if it takes a journey to different professionals to get the help you need just as I did herein my own journey.
At the end of this, I will know beyond a doubt what I can expect from the proposed Gastroc Recession Surgery and the possible ongoing need of the heel lift to give my shorter left leg all the help it needs to stop the demand of my pelvis/lumbar spine wanting to shorten/hike up my right hip via the Quadratus Laborum muscles to compensate for the longer right leg. I identify with the answer of this professional, Kate Simmons, myofascial pain specialist that wrote a reply to this question: “When I am walking, my right shoulder is somewhat lower in height than my left shoulder. What’s the solution to the above problem?” as linked at this site herein: http://www.quora.com/When-I-am-walking-my-right-shoulder-is-somewhat-lower-in-height-than-my-left-shoulder-Whats-the-solution-to-the-above-problem
All I can say to anyone reading this blog, there is no doubt on how the role of your feet and lower leg bio-mechanics plays into the pelvis and ultimately your back. Piece by piece this puzzle has been coming together. I feel like I am a detective in rooting out every last detail in order to walk what should be a normal gait. I am now continuing to inform other patients that have Sacroiliac Joint Dysfunction to now take a look at structural limb length discrepancy as a possible component in their situation. I’m always grateful to my Great Physician, Lord and Savior Jesus Christ for His inspiration that guides me to research and apply what I read to every detail of my rehabilitation process. And to the team of medical professionals He has given me to carry out His Will for me in finishing the race of bio-mechanical discovery and ultimate recovery in the process.
Please subscribe to my feedback form to get automatic notices of future blog posts.
Search for and Like SI-Instability.com on facebook!