 My current story on Subtalar Joint Instability starts with the diagnostic words, “Sinus Tarsi Syndrome” of my left ankle in March of 2013 given to me by my Champion Sports Medicine Physician, Dr. PZ Pearce, Spokane, WA. Now that the SI Joint Instability/Pain generator was eliminated after the successful SI-Fixation Surgery done 1-17-13, my attention was needed for my Proximal Tibiofibular Joint Instability and my left ankle pain. See my www.fibularpain.com for all the Proximal Tibiofibular blogs to date. And since I’ve also eliminated the Tib-Fib joint instability/pain issue of my left knee, I am now on my new medical journey with writing about my left ankle that has had issues for many years. Let the story begin!
My current story on Subtalar Joint Instability starts with the diagnostic words, “Sinus Tarsi Syndrome” of my left ankle in March of 2013 given to me by my Champion Sports Medicine Physician, Dr. PZ Pearce, Spokane, WA. Now that the SI Joint Instability/Pain generator was eliminated after the successful SI-Fixation Surgery done 1-17-13, my attention was needed for my Proximal Tibiofibular Joint Instability and my left ankle pain. See my www.fibularpain.com for all the Proximal Tibiofibular blogs to date. And since I’ve also eliminated the Tib-Fib joint instability/pain issue of my left knee, I am now on my new medical journey with writing about my left ankle that has had issues for many years. Let the story begin!
My prior chronological history pertaining to my left ankle or lower left leg is as follows:
Jan. 2002 – Foot Drop of left foot related to nerve compression due to massive herniation of L5-S1 (See MRI Image on Chronological Page of Website). The foot drop was resolved after my micro-discectomy surgery in April 2002.
April 2002-Jan 17-2013 – due to SI Joint Instability, bio-mechanical deficit/malalignment syndrome creating compensation patterns of left leg and ankle
Oct. 2010 – My horse stepped on my lateral foot near opening of Sinus Tarsi and also twisted my ankle. Other than the foot drop, and poor bio-mechanics for years, this was the only direct injury to this left ankle/foot. Due to ongoing pain and impingement over next months, I sought the help of Dr. Shirzad, Foot/Ankle Specialist with Northwest Orthopedic Specialists. After reviewing clean ankle x-rays, he proceeded to order an MRI with the possibility of Anterior-Lateral Impingement of my ankle.
June 29, 2011 – click here for MRI Lf Ankle 6-29-11
Aug. 31, 2011 – Successful Left Ankle Arthroscopic Surgery by Dr. Shirzad, see my 2 pages of surgical report for details.
Left Ankle Surgery 8-31-11, pg. 1
Left Ankle Surgery 8-31-11, pg. 2
I recovered after this surgery and could now dorsiflex my ankle so much better as the impingement was no longer there. Here is some patient to patient advice that I learned through the post-op process of the arthroscopic ankle surgery. It is important to be very careful during the first 24 hours and pay attention to the swelling of the ankle. Because I felt so good and I was allowed to bear weight immediately( I had no repairs, only debridement of joint) in a CAM walking boot, I did not notice the swelling building up in my foot. I could not feel pain against the side of my ankle up against the frame of the walking boot due to the Marcaine Injections into the ankle joint prior to waking up from the surgery. Because of pressure of the ace wrap and my ankle rubbing against the boot, I experienced a burning of my skin up the line of my distal fibula bone. I suffered with pain in this area over the next 3 weeks and no pain where the actual arthroscopic incisions were done or in the joint itself. If I had paid more attention, this could have been avoided so that is why I share it with others now. I know it is standard advice to not disturb post-surgical dressings for the first 3 days, but loosening an ace wrap needs to be done in addition to ice and elevation. The skin is so sensitive in a swollen state.
Since I was allowed to walk to tolerance, of course I took full advantage as I was not a couch potato. I do have a high tolerance to pain and that is why I can do more than say someone else. But after the fact, I would have done things differently. I would not have walked on ankle/foot right away even with the CAM boot. If it had been my choice, I would have chosen a molded posterior splint to keep ankle at 90 degrees and stay non-weight bearing for the first 3 days then transitioned into a walking boot and tennis shoes later on. As it turned out, I had to use the walking boot for almost 3 weeks before I could get into tennis shoes. Just my food for thought!
May 2, 2012 and Sept. 25, 2012 – To deal with nerve pain of my left lower leg and foot, I had two surgeries. For these details, please see my peripheral nerve surgery blog that discusses the decompression surgeries for the Common Peroneal, the Superficial Peroneal, the Deep Peroneal and the Proximal Tibial Nerves of my left leg. I spent the better part of the year 2012 doing physical therapy and recovering very well from these 2 surgeries. My nerve pain was eliminated but I continued to have some ankle issues.
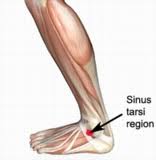
 So in March 2013 when Dr. PZ Pearce palpated my foot and said I had symptoms of “Sinus Tarsi Syndrome”, I certainly did not know what he was talking about. The red circle of this photo shows the exact area of my predominate point of pain Even though I had studied many ailments of the ankle prior to my first surgery, I had never looked up this diagnosis before as I simply never heard the words until this time. I quote the following from author Bruce Lashley, DPM with a link to his article “Treatment of Sinus Tarsi Syndrome”:
So in March 2013 when Dr. PZ Pearce palpated my foot and said I had symptoms of “Sinus Tarsi Syndrome”, I certainly did not know what he was talking about. The red circle of this photo shows the exact area of my predominate point of pain Even though I had studied many ailments of the ankle prior to my first surgery, I had never looked up this diagnosis before as I simply never heard the words until this time. I quote the following from author Bruce Lashley, DPM with a link to his article “Treatment of Sinus Tarsi Syndrome”:
” Where and what is the sinus tarsi:
The word “sinus” refers to a cavity, most often in bone. The cavity known as the sinus tarsi is located on the outside of the foot in front of and below the outside anklebone. The cavity is formed at the junction between the heel bone and the bone that sits over the heel bone called the Talus. The heel bone forms the floor of the cavity and the talus creates the roof.
Within the cavity there are blood vessels, nerves and ligaments. The ligaments function to hold the two bones together.
Symptoms:
“Sinus Tarsi Syndrome” refers to a painful condition located in this cavity in the rear portion of the foot. The pain is made worse with weight bearing. The pain can become much more intense when walking, running or hiking on uneven surfaces.”
Dr. Lashley’s entire article is very important to read as I only quoted a portion above so my readers can understand what part of the anatomy I’m talking about. Yes my pain increased with walking and would just about be gone after having a good night sleep. I identified with Dr. Lashley’s article.
I came across another one of my favorite articles on the subject written by Jeffrey A. Oster, DPM at www.myfootshop.com. Here is the link to his article on Sinus Tarsi Syndrome. I quote from Dr. Oster’s article the following:
“Most doctors who work with the foot and ankle believe that sinus tarsi syndrome is due to repetitive traumatic load applied to the subtalar joint resulting in forced inversion of the joint. Examples of repetitive inversion activities that would injure the subtalar joint include the trailing foot of a softball pitcher or bowler. Other examples include sitting with the feet tucked under the weight of your body. Each of these activites results in forced inversion of the subtalar joint and strain on the sinus tarsi.“
In my case, I certainly sat for years with my left foot tucked under the weight of my body while doing office work. This was especially pronounced after I recovered from the nerve interference of the prior foot drop which had caused a residual excessive plantar flexed position of my left foot while in a relaxed state. Dr. Oster went on to say in his Sinus Tarsi Syndrome article and I quote:
“Treatment of sinus tarsi syndrome begins with identification of the activity that may be contributing to subtalar joint injury. Rest and bracing of the subtalar joint, using an ankle brace is helpful. Orthotics do help to limit the range of motion of the subtalar joint.”
I was already using custom made orthotics for over a year and I did continue trying several different ankle braces that were recommended on Dr. Oster’s website: www.myfootshop.com Nothing seemed to bring any lasting measure of relief except being wrapped in sports tape, coban and/or 3M Soft Cast Casting tape along with doing my own trial of non-weight bearing after a chiropractic adjustment. Armed with some insight, I proceeded to get a second opinion on whether or not I had Sinus Tarsi Syndrome from Dr. Ronald Alm, DPM a more local foot doctor in Lewiston, ID to verify what my sports doctor in Spokane was trying to tell me.
March 27, 2013 – New patient appointment with Dr. Alm, DPM and my examination findings: “examination reveals she is quite tender over the sinus tarsi LEFT, mild tenderness over the peroneal tubercle…She does have symptoms in the area of the superior tib-fib complex with maximum dorsiflexion of the ankle. In stance she does have a slightly pronated foot structure with a decreased arch, she does have a slightly inverted heel and rectus forefoot.” His impression was: “Unstable superior tib-fib complex, sinus tarsi syndrome left and forefoot valgus bilateral.” He advised me to continue with my current treatment program with my sports medicine physician and my chiropractor. He added a forefoot valgus post to my left custom orthotic to help balance my foot under my metatarsals to help ease some pressure along the lateral column which did give a measure of comfort to my foot and to see him again as needed. Dr. Alm suggested a possible future diagnostic Cortisone injection into the opening of the Sinus Tarsi. I certainly wanted to wait as I avoid Cortisone at all costs unless absolutely necessary.

April 2013 – During this month, I continued in many appointments with my sports doctor and extremity adjustments with my chiropractor, Dr. Sheldon, DC. In the meantime, my ankle always seemed to pass any of Dr. Shirzad’s or Dr. Alm’s standard ankle stability tests but my ankle still needed constant adjustments by the chiropractor.
My goal at this time was to figure out whether my Superior/Proximal Tib-Fib joint or my ankle or both were the source of my pain generators. Here is photo of me at this time with my ankle and leg wrapped for support to ease the pain I felt on a daily basis. I really did work hard at paying attention to every detail of what made me feel better and what made the pain worse. The conclusion became clearer that the Proximal Tib-Fib joint was worse off/more unstable than the ankle so I pursued dealing with my Proximal Tibiofibular Joint first. The hope was to stabilize it and see if the ankle pain would also calm down. I choice to temporarily set aside dealing further with the Sinus Tarsi Syndrome and I proceeded on 5/14/13 with surgery on my Proximal Tibiofibular Joint.
My ongoing ankle story picks up again in July 2013 when I start walking again after my non-weight bearing post-op status for the Tib-Fib surgery. See my next blog.
Or just subscribe to this blog (right sidebar) to receive automatic updates whenever I post a blog story about my medical and spiritual journey.

