From my last Piriformis Syndrome blog posted July 23, 2013, I wanted to give an update and where my journey has taken me on this subject. It wasn’t until November 2014 that I revisited this subject amongst all that I had been doing to stabilize my lower extremities with HyProCure Surgeries and Proximal/Distal Tibiofibular Joint Surgeries. From July 2013 till Sept. 2014, I had managed pretty well with only minor flareups even though I had to do a lot of sitting with all my post surgery rehab times. But in September when I went riding on my horse for a 2 hour trail ride, I ended up with a major flareup of localized pain behind my Greater Trochanter of my left hip. This time it was not really bad nerve pain down the leg but a more localized feeling of something torn. It was miserable to lay on that hip for the first time in my life and that is when I went to my pain doctor, Dr. Patrick Soto, for the first time since the spring of 2014.
October 21st, 2014 – Dr. Patrick Soto spent time in hearing my updates of my progress since SI Surgery and my lower extremity surgeries. He was pleased with my progression and heard my concern regarding my ongoing issues in my left glute muscle insertions and/or hamstring insertion. He felt very strongly that I would benefit from the services of another doctor that specialized in ultrasound guided injections for which he did not do. He specialized in more traditional fluoroscopic guided spine injections and pain pumps and was now working more with acute/trauma cases than chronic cases. So he personally referred me to Dr. Katrina Lewis and with a cancellation I was able to see her the very next day.
October 22, 2014 – My first visit with Dr. Katrina Lewis, The Pain Clinic of Spokane, who specializes in Ultrasound Guided PRP (Platelet Rich Plasma) injections along with all the more traditional spinal injections and pain management. Dr. Katrina Lewis took an interest in all that I had been through thus far in my history. Before we jumped ahead to doing any injection therapy, she wanted me to see a specific pelvic floor trained physical therapist during the next month before returning to her in order to rule in or out Obturator Neuropathy.
Oct 28th, 2014 – Initial Evaluation with Christy Frazier, DPT at Apex Physical Therapy. Her findings: “Tension in medial thigh, right lower extremity longer mildly and tighter psoas muscle. Palpation: Left medial thigh fascial restrictions, tightness to stretch but no pain to pressure. Bilateral piriformis tension and left gluteus medius tension. Mild tenderness to left obturator internus but non-tender to all other pelvic floor muscles assessed externally. Assessment: “Kim is experiencing signs and symptoms consistent with left medial thigh fascial restrictions which could be related to gait pattern. Her symptoms also suggest obturator neuralgia but she was negative for all pelvic floor external palpation and further internal PF investigation will be performed at next appointment.”
November 5th, 2014 – Christy Frazier, DPT after doing an internal pelvic assessment: “Negative for all testing for obturator neuralgia. No notable pelvic floor tension or pain. She does have fascial restrictions right medial thigh and left lateral achilles area. I do think she would benefit from further fascial mobility treatment with gua sha tools…”
November 25th, 2014 – Christy Frazier, DPT assessment: “Kim is no longer reporting medial thigh tension and burning pain and I think this is directly related to altering her gait pattern. She does not seem to have any Pudendal or Obturator nerve involvement from the testing I’ve performed and I think with improved length in her left Achilles tendon she will have the potential to permanently improve her gait pattern leading to less thigh and hip dysfunction.”
I also had a follow up appointment this day with Dr. Lewis to share with her my physical therapist’s findings and to let her know that back on Oct 28th, 2014 after seeing her last, I did have my limb length discrepancy x-ray done and I finally found out that I had a 4mm shorter left leg. The full story is written in my blog in the Short Leg Syndrome category of this website.
So through the process of learning and discovery and not giving up hope, I was able to find the source of my fascial flareups with sensory burning symptoms. They had a direct relationship to my walking gait and how it has been compromised by my structurally shorter leg and my restricted Gastroc/Soleus-Achilles tendon issue in my lower left leg. Regarding the pointed spot of tenderness near my hip, it happened as a direct result of over pulling my left leg down in my saddle on the 2 hour ride back in September to make it feel longer or equal to my right leg before I knew it was truly structurally shorter. So I wanted to proceed with a PRP injection into my hip area to help heal this sore region while I would be simultaneously taking it easy after going to have my Endoscopic Gastroc Recession Surgery on 12-30-14 to lengthen my Achilles Tendon and to get normal dorsiflexion back to my left ankle.
 December 17th, 2014: I went into the clinic with complaints of tenderness in my left subgluteal region, possibly at the insertion of the hamstrings, that I thought might have some chronic tendinopathy or bursitis causing persistent pain. Dr. Katrina Lewis through her ultrasound guidance skill was able to find an area with some mild fluid and/or tendinopathy around the ischial bursa region as well as the hamstring insertion. She performed a PRP(Platelet Rich Plasma) injection into this area. The injection really was not painful at all in this part of the body. Just some localized bruising afterwards.
December 17th, 2014: I went into the clinic with complaints of tenderness in my left subgluteal region, possibly at the insertion of the hamstrings, that I thought might have some chronic tendinopathy or bursitis causing persistent pain. Dr. Katrina Lewis through her ultrasound guidance skill was able to find an area with some mild fluid and/or tendinopathy around the ischial bursa region as well as the hamstring insertion. She performed a PRP(Platelet Rich Plasma) injection into this area. The injection really was not painful at all in this part of the body. Just some localized bruising afterwards.
Dec. 30th, 2014 – Here is link to my Endoscopic Gastroc Recession Surgery
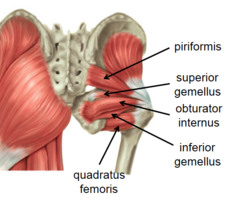
January 21st, 2015: This was a follow up appointment to my last PRP injection. Dr. Lewis performed another ultrasound exam while I was in a prone position and described her findings as follows: “We started by examining the subgluteal area first. At the ischial bursa, I have noted some fluid suggestive of continued bursitis. Hamstring insertion muscles appeared normal. The sciatic nerve looks as though it is right up by the piriformis muscle, possibly within it which may be causing a significant amount of the patient’s symptoms. No obvious nerve swelling or adhesions are noted. I have suggested that we could inject some saline around the nerve to release it from the piriformis. This would allow us to know whether or not there were any adhesions in that regard. Gluteus medius looks fine; however, the piriformis does not look as uniform as the gluteus medius. The fascia looks irregular at the attachment to the greater trochanter. The medial part of the piriformis does appear intact and the fibers appear normal. Along the attachment of the quadratus lumborum along the iliac crest there is evidence of enthesopathy. ”
After this appointment with Dr. Lewis, I began my walking rehabilitation journey from being non-weight bearing for 3 weeks since the Endoscopic Gastroc Surgery. I spent the months of February and March focusing on my lower leg rehab. When I felt like I was walking the best I could, I then went back to Christy Frazier, DPT for a recheck on my fascial condition of my inner thighs. My glute muscles themselves were feeling very good with the newly found balanced walking gait. I also wanted to revisit Dr. Soto who also did Osteopathic Manipulations(OMT) and get his take on my current lumbar spine condition.
March 31st, 2015 – Dr. Soto’s objective findings: “Increased tone in the right lumbar paraspinals. L5RrS1. Linea alba tight with decreased lower rib excursion and diaphragm restriction bilaterally.” Procedure: OMT, muscle energy and direct myofascial release utilized to the lumbar and abdominal regions with correction of the L5 rotation and improvement in the abdominal region. He also gave me an additional referral to another up and coming doctor in the area specializing in Osteopathy with specific training in the Cranial Field along with body bio-mechanics and Prolotherapy to see if this could benefit my lumbar spine. He advised against using my back brace on a regular basis for my sense of instability of my lumbar segments. He congratulated me on my significant progress to date and for my active participation in my care.
April 1st, 2015 – Since leaving off with Christ Frazier, DPT in December 2014 before my Gastroc Surgery, this day I saw her again for the first time and her observations this day: “Limited right trunk rotation with gait, tension in right diaphragm, limiting right rib expansion with inhale.” She did her manual therapy of a right diaphragm release and what a difference it made when I walked again for her after the therapy. It was amazing to see how restrictions in the diaphragm/ribs do affect the lumbar. She had already commented on how well I was maintaining neutral pelvis with my gait pattern and she was so happy for me that the Gastroc/Achilles lengthening surgery had been a success. I walked out of the clinic with renewed hope on sorting out what I call little details compared to the whole picture of my entire journey thus far; however, these little details do make a world of difference in bio-mechanical function of our spine.
April 15th, 2015 – Another appointment with Christy and she was pleased to find that I had applied what she taught me in breathing and mobilizing my lower ribs. She observed: “Almost no right diaphramatic tension and good trunk rotation with gait pattern, appropriate ankle rockers taking place and good pelvic positioning today. Left medial hamstring fascial restriction present and left calf tension.” She also did manual therapy on my left hamstring fascial symptoms.
April 22nd, 2015 – Christy Frazier, DPT Assessment:” Only a few points of fascial restriction still present in left medial hamstring. Gait pattern continues to look symmetrical. Joint positioning in thoracic and lumbar spine seems WNL with movement.” Christy showed me how to roll over a small ball to help my thigh fascia when it gets tight and I have continued to do that.
![]() I saw Christy one more time on 5-11-15 and she released me to maintain myself with home exercise because I had accomplished the goals set for me. I felt really good at the accomplishments and was pain free in my glutes and only some intermittent fascial tightness which gives a sensory burn feeling that continues to respond very well to rolling it over a small ball. She also recommended that I buy the TheraBand Roller Massager as pictured on the right available on Amazon. The insertions of the piriformis and glute medius behind my left Greater Trochanter were by this time feeling so much better and no more sharp pain. I was able to now sleep on that side at night. The PRP injection did help the healing along with the positive bio-mechanical changes.
I saw Christy one more time on 5-11-15 and she released me to maintain myself with home exercise because I had accomplished the goals set for me. I felt really good at the accomplishments and was pain free in my glutes and only some intermittent fascial tightness which gives a sensory burn feeling that continues to respond very well to rolling it over a small ball. She also recommended that I buy the TheraBand Roller Massager as pictured on the right available on Amazon. The insertions of the piriformis and glute medius behind my left Greater Trochanter were by this time feeling so much better and no more sharp pain. I was able to now sleep on that side at night. The PRP injection did help the healing along with the positive bio-mechanical changes.
During this time I simultaneously continued also with my Postural Restoration Institute Trained Physical Therapist-Mark Bengtson, MPT at Pinnacle Physical Therapy as he was in charge of my lower left leg rehab on behalf of my surgeon, Dr. Gent-Kitsap Foot and Ankle Clinic of Bremerton, Wa. I also continued with my personal trainer/yoga instructor, Joanna Alford, MPT at my home and she continued to also monitor my walking outside my home. And I had full-body medical massage weekly. With all of this help, I made tremendous progress in my lower leg, hips and thighs and increased more stability in my entire spine.
May 10th, 2015 – A VERY HAPPY MOTHER’S DAY WITH MY DAUGHTER ALLY (as pictured here, it was so great to be comfortable while standing in heels)
May 11th, 2015 – I finally was able to have an appointment with Dr. Philip Lenoue, III DO, at Lenoue Integrative Medicine in Spokane, WA that Dr. Soto had referred me to. This doctor was basically coming into my journey to add what I call more icing to the cake. He found my website very interesting, complemented me on all my success, and then wondered what he could now do for me. I told him to give me a once over just like he would initially evaluate any other patient. He proceeded to do his Cranial Osteopathic Therapy as he is a member of The Osteopathic Cranial Academy. He warned me that most patients will have increased pain after his therapy (even though his therapy was more subtle than any prior chiropractic treatment), but to drink a lot of water and pain would subside. Well he wasn’t kidding, as I walked out of there with a headache that finally subsided after more water and dinner. I never got any headache from chiropractic care or physical therapy. He surely did something different but I cannot put into words what he did. He also did some kind of mobilization to my abdomen.
He came right out and asked if I had any prior trauma to my head from whatever his trained hands were picking up. Yes I was pulled into this world with forceps back in the 60’s, my forehead hit the steering wheel in a car accident at 17, and I was whip lashed and thrown from a horse landing on the base of my neck in a field when I was in my early 30’s, and then my last whiplash landing on my back in arena at age 50. He also checked over my left forearm and wrist tendons, and a check on my peroneal tendons which have been bothering me in my left foot. I asked if he wanted to see my recent wrist MRI and he said no. He relies on more hands on than diagnostic imaging. He thought I could benefit from prolotherapy in my left forearm Annular Ligament and others too because I told him I felt like I had instability of both my proximal and distal radioulnar joints. I will be writing future blogs on the subject of my left arm/wrist.
I really must say I owe another debt of gratitude to my Dr. Soto. In his wisdom and with humility, he referred me on to another doctor that he believed could further help me with OMT and especially with prolotherapy. It will take awhile to see Dr. Lenoue again due to scheduling as he is busy finishing his family residency at a local hospital along with taking on new patients in private practice. In the meantime, I left Dr. Lenoue’s office feeling like God had given me another special blessing of a doctor with skilled hands and a knowing of what soft tissue structures are suppose to feel like and when it is compromised. He learned early on about hands on therapy as he grew up with a father that is a Chiropractor.
SUMMARY:
Piriformis Syndrome is real and it usually is a secondary condition related to malalignment of SI joints unless there is a direct injury to the hip/or the muscle itself. Provocative EMG testing as shared in my first Sacroilac Joint Surgery blog is a very important test along with the ultrasound to see the condition of the tendon insertion and position of the sciatica nerve. The muscle gets tight and spastic due to its nature to protect the SI joints. Here is a link to research article regarding Sacroiliac Dysfunction and Piriformis Syndrome: http://www.sidysfunction.com/pdfs/Medical-Piriformis.pdf
When its tight and spastic, then welcome in piriformis sciatica. Piriformis sciatica may be similar but usually differs from lumbar radiculopathy/sciatica as it is less dermatomal specific and usually the nerve symptoms are more diffused within the buttocks and thighs and not necessarily radiating to the feet but in severe cases it does radiate to the feet as mine had done many times with too much sitting in the past. Here are some good links to Sciatica.org: http://www.sciatica.org/piriformis/index.html
http://www.sciatica.org/piriformis/differential_diagnosis.html
Here is a link to a wonderful and comprehensive blog that I follow of a man that had piriformis syndrome not related to Sacroiliac Joint Dysfunction: http://piriformissyndrome.me/
MY PERSONAL SUMMARY:
This blog finishes my piriformis category subject for this time on my website. I now know what I’m left to deal with which is really nothing at all as I am truly pain-free. Compared to many patients out there that are suffering continually with piriformis syndrome in relationship to their SI Joint Dysfunction, I just need to be careful and nurture my tendon insertion of my left piriformis into my Greater Trochanter, and maintain good body bio-mechanics that I’ve achieved over the last 2 years. If I need any further PRP injections into the piriformis or gluteus tendons or saline injections around sciatica nerve, I will pursue Dr. Katrina Lewis to take care of these for me. I will pursue Dr. Lenoue for prolotherapy if needed to help my lumbar ligaments or any ligament laxity issues throughout my body.
May 24th, 2015 – As I have put in more than 8 hours of sitting time today to type this blog, I have no nerve symptoms in my legs, no burning butt pain, no lumbar spine pain, no neck pain. I am more flexible than ever with all the muscle spasm gone from my body. What can I say, I’ve worked hard to achieve symmetry in my body; rid myself of Mal-alignment Syndrome with stabilized bi-lateral SI joints along with stabilized bi-lateral Proximal & Distal Tibiofibular joints and Subtalar joints through minimally invasive surgeries. I use a foot lift to balance the 4mm of shortness of my left leg, and I do regenerative PRP Injections.
June 28th, 2015 – I needed to take some time between doing the draft of this blog and sitting down to finish it off for sure. I’ve been busy regarding my lower left leg rehab, peroneal tendon PRP injections/rehab and analyzing the remaining details of my left arch. I will write an update about all that here shortly in its own category-Short Leg Syndrome. I also had a set back with an injury to my horse over the past week that I’m dealing with. I’ve been busy with answering emails and calls to my website. There is a world of hurting patients out there and I’m just trying to do my part in being a helping hand. In the meantime, I have enjoyed more swimming and a few more times of dancing and a couple of times on my horse. I still stand amazed at the quality of life I now have as though I never ever had the piriformis syndrome for so many years prior.
To God be the Glory for His Mercy and Wisdom in my life and to my team of medical professionals that have come alongside to give me the best of their care. I pray for all patients out there that read my blogs and for those that reach out and contact me. Never give up hope for answers to your prayers!
Stay tuned by subscribing to my website in the subscription box or see and like me on Facebook. Also any patients that have been helped through this website are more than welcome to submit a comment that I can publish for my Patient Endorsement Corner.

