This blog is my rehabilitation from my left leg Endoscopic Gastrocnemius (Gastroc)/Soleus Recession Surgery starting at 3 days post op with PRP injections and working my way through till 6 weeks of recovery. It was very challenging from 3-6 weeks as I did my physical therapy and I walked while working through pain; however, the surgery was nothing short of a miracle to give me the ability to walk normal. My last blog features the surgical report and Endoscopic photos.
Jan. 2nd, 2015 – Starting the New Year at my 3-day post surgery appointment with Dr. Gent, DPM of Kitsap Foot and Ankle Clinic, Bremerton, WA. Here are pictures of my surgical sites on my left leg. (Click on photos to enlarge)
As you can see from the photos very minimal swelling. The black patches on my leg were the leads for my TENS unit for pain control. I never took any narcotic pain medication after the surgery. Only 2 times a dose of 1000mg of Tylenol and a few nights of Flexeril muscle relaxant. Here is my YouTube video of Dr. Gent explaining how well I was doing after the surgical splint was removed.
Dr. Gent did Platelet Rich Plasma (PRP) injections into my left leg medial surgical site. He also gave me a boost to my right ankle ligaments and joint space with the remaining PRP as I never had this done on my right ankle before. He allowed me one moment of standing up on my right leg with my husband holding me so I could just touch down my barefoot left leg to the floor in order for me to feel the difference of the new length my calf now had from the surgery. It certainly was a hopeful and joyous moment. Then Dr. Gent proceeded to put a short leg fiberglass cast on my left leg. He took his cast saw and bi-valved the sides of the fiberglass to allow for swelling. My ankle needed to be held at 90 degrees and to give the back of my gastroc and soleus muscles time to heal with non-weightbearing (NWB) for 3 weeks. Here is my Youtube video showing final cast.
I left Dr. Gent’s office with my knee scooter happy to embrace the next few weeks of NWB. I so desperately wanted success and he encouraged me to call him with any concerns along the way. I did well for the 7 hours in the car back to Idaho. Over the next two weeks, I had thought this surgery was a piece of cake compared to all my other surgical experiences. No pain, no icing just elevation of my leg in the evening before bed. Little did I know what would be next when it was time to bear weight.
January 19th, 2015 – I just had the stitches taken out by my local DPM, Dr. Alm and I transitioned into my walking boot now that I was 3 weeks from surgery. Dr. Alm stated that my incisions looked good and to continue following the advice of my surgeon, Dr. Gent. I still was to wear the Bi-valved fiberglass cast at night to continue keeping the stretch of my Achilles and ankle at 90 degrees. In fact my leg had been very comfortable in the cast the entire past 3 weeks and no problems with sleeping.
January 20th, 2015 – My first physical therapy appointment with Mark Bengtson, MPT-Pinnacle Physical Therapy, Post Falls, ID. Here is my YouTube video of my leg with Mark doing manual therapy. At first my leg was hyper-sensitive to his touch, but it quickly came to appreciate his therapy.
January 22nd, 2015 – Phone consult-Dr. Gent reviewed the video I had made of my first physical therapy appointment and he was extremely pleased with how well I was doing on my leg. In my case, he encouraged me to transition out of the walking book as tolerated over the next week; however, it was imperative that I keep the cast on at night which I was happy to do because my leg did feel so supported and comfortable. Now looking back, I could see why Dr. Gent insisted on a cast and not immediate weight-bearing in a walking boot after this surgery whereas some doctors do allow their patients to have weight-bearing as tolerated in a walking boot after this surgery. The cast protected my muscle to allow the surgical slice of the Aponeurosis to heal/scar down and keep me from getting a Hematoma which would have been more painful. MedicineNet.com definition of Hematoma: “A localized swelling that is filled with blood caused by a break in the wall of a blood vessel. The breakage may be spontaneous, as in the case of an aneurysm, or caused by trauma. The blood is usually clotted or partially clotted, and it exists within an organ or in a soft tissue space, such as muscle.” Also I can attest that my calf muscles were not ready to have my standing weight on them up until this 3 week point in time.
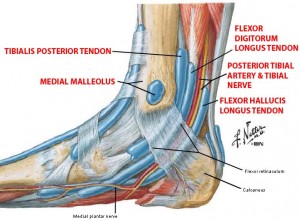
January 23rd, 2015 – This was a horrible night for me. I had now been in the walking boot 5 days with pain in my heel from day one of walking. And now this night, I felt like I had ripped my Posterior tibial tendon area above my medial malleolus as it was on fire. Thank God my massage lady had come over and she helped to calm this down. I called my physical therapist the next morning and he encouraged me to make ice cups and direct ice this area several times a day. The next day I stopped the walking boot because it was just too hard on the bottom of my foot and I transitioned into my tennis shoes with a double layered ace wrap up my leg for support.
I was keenly aware that the deep posterior muscles(Tibialis and Flexors) were in need of rehab right along with the Gastroc and Soleus. After all, they needed to stretch now too to go along with the new length of the Gastroc/Soleus complex. I wanted everything to be fine in a week’s time of walking. Yeah right! Who was I kidding.
Over the next two weeks, I got new OTC Powerstep brand of orthotics, heel cups and switched back and forth with different tennis shoes to be comfortable while walking. I worked hard at paying attention to what would flare my foot/heel pain during the day because it would go away at night. I started using my Infrared heating pad to increase circulation to my muscles before my daily ritual of stretch band exercises and then my evening ritual if icing and elevation of my leg.
February 9th, 2015 – I went back to Dr. Alm for him to do a hands on exam in order that I would have information to share with Dr. Gent with his findings. Dr. Alm’s impression: “Mild tarsal tunnel syndrome with superficial and deep posterior muscle pain” Dr. Alm explained that the Tibial nerve has a branch going under the heel and the swelling around the Tarsal tunnel area compresses the nerve and creates the heel pain.
Feb. 11th, 2015 – I am now 6 weeks since surgery and I’ve been exercising and walking now for 3 full weeks. Here is my home physical therapy video discussion/ sharing the details narrated by Joanna Alford, MPT/Yoga Instructor of where I still had pain to present to Dr. Gent. By this time, the bottom of the heel pain was much better under control .
Feb. 12th, 2015 – Phone consult with Dr. Gent and he appreciated the detailed video of my leg and my concerns. It helps to share videos because it is too far to travel for regular post surgery followup. We had a nice discussion and he ordered Iontophoresis to be done around my ankle to calm the sensitive Posterior Tibial Tendon and the Musculotendinous junction of my Achilles. My physical therapist set me up with a home unit to administer a transdermal patch dose of Dexamethasone into these areas over the next 6 days.

Feb. 15th, 2015 – I had been using the Rodeo Core exercise equipment. For those interested, search for the YouTube video of the product. I liked the active yet gentle workout it gave me and helped to tune my muscle strength up for riding again after being laid up with my lower leg. It also felt good as a partial weight-bearing exercise to push through my lower legs. It also was nice to jump on it after sitting in my office chair to bring mobilization to my lower back and build core strength. My actual walking time was increasing as pain subsided from my lateral Achilles and my Posterior Tibial Tendon around medial ankle. I just had my first swim this past week since last fall. I’m looking forward to steadily increasing all my activity. I’ve been back on my horse for 2 times say 15 minutes each these past two weeks. I was still weak getting on my tall horse and I needed help to get on an off; however, I certainly did not have any problems doing all 3 riding gaits while putting pressure to side of my leg. A little weak in my lower back because I now was readjusting to two even legs in the stirrups. It certainly was a positive bio-mechanical change up my entire being after this last leg surgery and I now need to retrain certain low back/pelvis muscles to not try and shorten up my former longer right leg and twist my lower back. I just need more time in the saddle.
My next blog will continue the story of the progression of my healing and increased walking. I close this blog knowing that I was only 6 weeks since surgery and my past experience has always proved that each week will get better. Stay tuned!



